
Source: FDA.gov

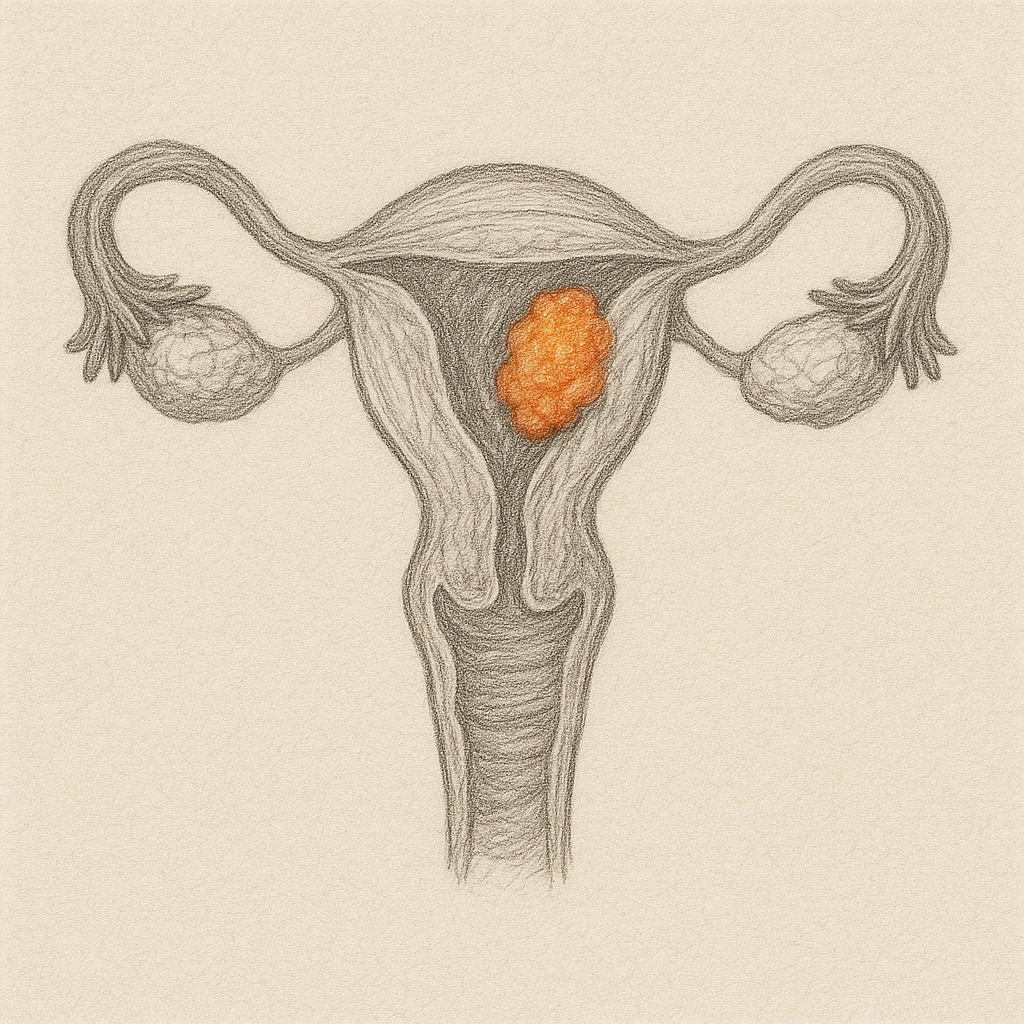
The FDA approved pembrolizumab combined with carboplatin and paclitaxel for advanced or recurrent endometrial carcinoma, providing the first immunotherapy-based frontline option for this patient population. This approval addresses a significant unmet need, particularly benefiting patients with mismatch repair deficient (dMMR) tumors who demonstrated exceptional progression-free survival outcomes.
Study Design & Population
- Study Type: Multicenter, randomized, double-blind, placebo-controlled phase 3 trial (KEYNOTE-868/NRG-GY018)
- Sample Size: 810 patients with advanced or recurrent endometrial carcinoma
- Cohorts: 222 patients with dMMR tumors; 588 patients with pMMR tumors
- Randomization: 1:1 to pembrolizumab + chemotherapy vs placebo + chemotherapy
- Stratification: MMR status, ECOG performance status, prior adjuvant chemotherapy
Key Findings
- dMMR Cohort PFS: Median not reached (95% CI: 30.7 months to NR) with pembrolizumab vs 6.5 months (95% CI: 6.4–8.7) with placebo (HR 0.30, 95% CI: 0.19–0.48, P<0.0001)
- pMMR Cohort PFS: 11.1 months (95% CI: 8.7–13.5) with pembrolizumab vs 8.5 months (95% CI: 7.2–8.8) with placebo (HR 0.60, 95% CI: 0.46–0.78, P<0.0001)
- Safety Profile: Consistent with known pembrolizumab + chemotherapy toxicities, with higher incidence of rash noted
- Dosing: Pembrolizumab 200 mg every 3 weeks or 400 mg every 6 weeks for up to 24 cycles
Clinical Implications
- Establishes first-line immunotherapy standard for advanced/recurrent endometrial cancer across MMR status
- Particularly transformative for dMMR patients with dramatic PFS benefit (70% reduction in progression risk)
- Provides meaningful benefit for pMMR patients (40% reduction in progression risk) where treatment options are most limited
- Expands pembrolizumab’s already extensive oncology portfolio to include frontline endometrial cancer treatment
Limitations
- Primary endpoint focused on PFS rather than overall survival
- Higher incidence of rash compared to previous pembrolizumab studies requires monitoring
- Long-term toxicity data from extended treatment duration (up to 24 cycles) still maturing
- Cost-effectiveness considerations for broader patient population, particularly in pMMR subset



