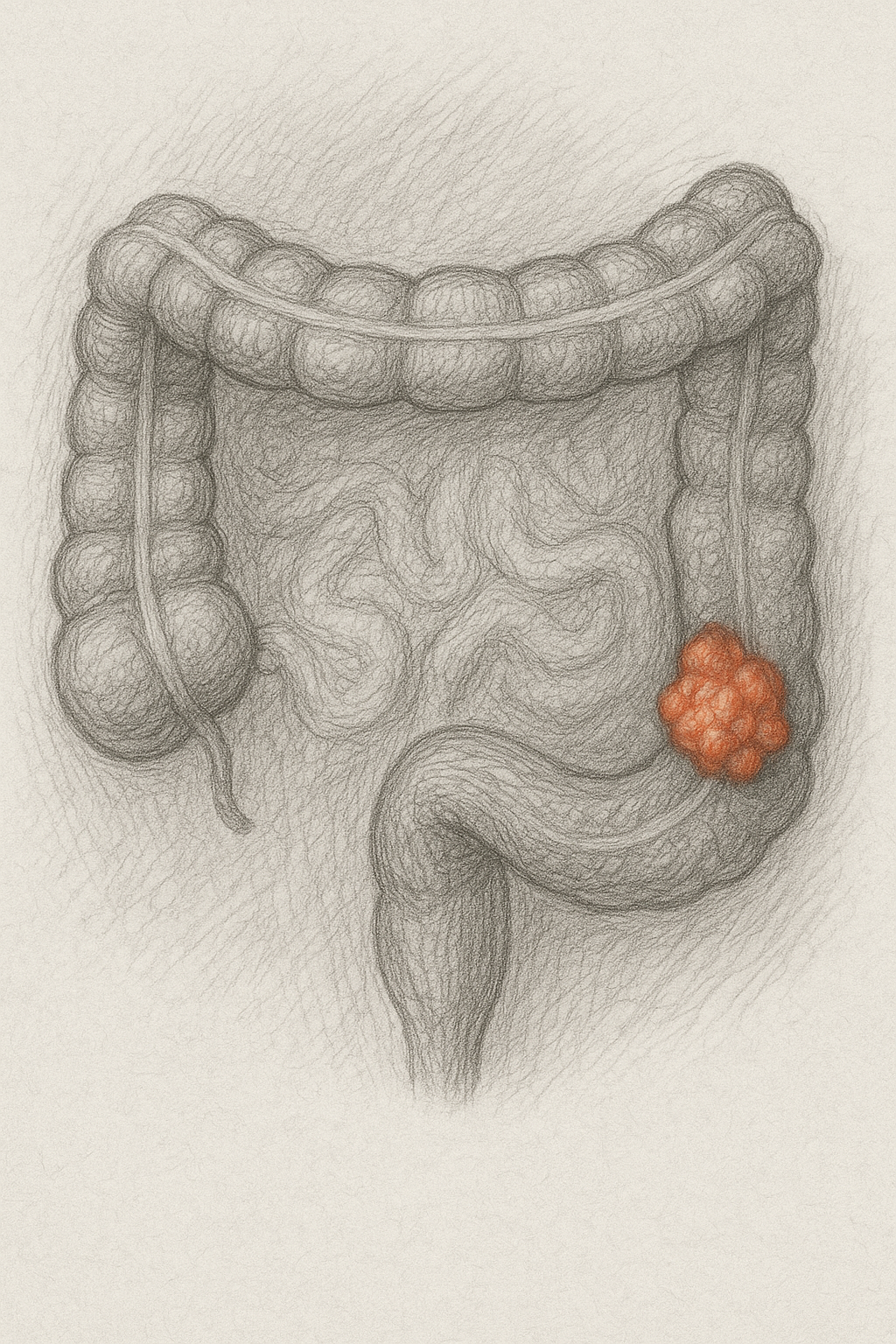

Colorectal cancer (CRC) screening among adults aged 45-49 years increased significantly from 20.8% in 2019 to 33.7% in 2023 following updated screening guidelines, with the largest gains in stool-based testing (5-fold increase). However, screening improvements were predominantly limited to higher-educated and insured populations, potentially widening health disparities.

Study Design & Population
- Cross-sectional trend analysis using National Health Interview Survey data
- Sample size: 18,645 (2019), 17,300 (2021), and 17,293 (2023) adults aged 40-75 years
- Target population: Adults aged 45-49 years (14.8%, 13.9%, and 14.0% of samples respectively)
- Demographics: Primarily White, privately insured participants
- Survey periods: Before (2019), during (2021), and after (2023) updated USPSTF recommendations
Key Findings
- Overall screening uptake increased 62% (APR 1.62; 95% CI 1.44-1.83) from 2019 to 2023
- Colonoscopy screening rose from 19.5% to 27.7% (APR 1.43; 95% CI 1.26-1.62)
- Stool-based testing showed dramatic increase from 1.3% to 7.1% (APR 5.37; 95% CI 3.36-8.57)
- College graduates: screening increased from 24.0% to 39.4% (APR 1.66)
- Privately insured: screening rose from 21.6% to 36.6% (APR 1.70)
- No significant change in screening rates for uninsured or less-educated populations
- Screening rates remained stable in older age groups (50-75 years)
Clinical Implications
- Early screening adoption demonstrates successful guideline implementation for younger adults at increased CRC risk
- Stool-based tests may be driving accessibility improvements and patient preference
- Health disparities persist and may be widening, requiring targeted interventions for underserved populations
- Healthcare system capacity appears adequate as older adult screening rates remained stable
Limitations
- Self-reported data subject to recall bias and social desirability bias, likely overestimating actual screening rates
- Survey response rates declined from 59.1% (2019) to 47% (2023), introducing potential nonresponse bias
- Cannot distinguish routine screening from diagnostic colonoscopies in primary analysis
- Sparse data in subgroups limits interpretation of disparity trends
- Claims data typically show lower screening rates than survey data
Source: https://jamanetwork.com/journals/jama/fullarticle/2837231