
Source: Journal of Clinical Oncology
URL: https://ascopubs.org/doi/10.1200/JCO.2025.43.16_suppl.5092

PSA nadir <0.2 ng/mL within 9 months of starting ADT-based therapy is the optimal target for mCSPC patients, conferring 54% lower risk of death and 55% lower risk of progression. The commonly used ≥90% PSA decline benchmark provides only modest survival benefit (22% death reduction) and no progression benefit, suggesting clinicians should prioritize absolute PSA values over percentage reductions.
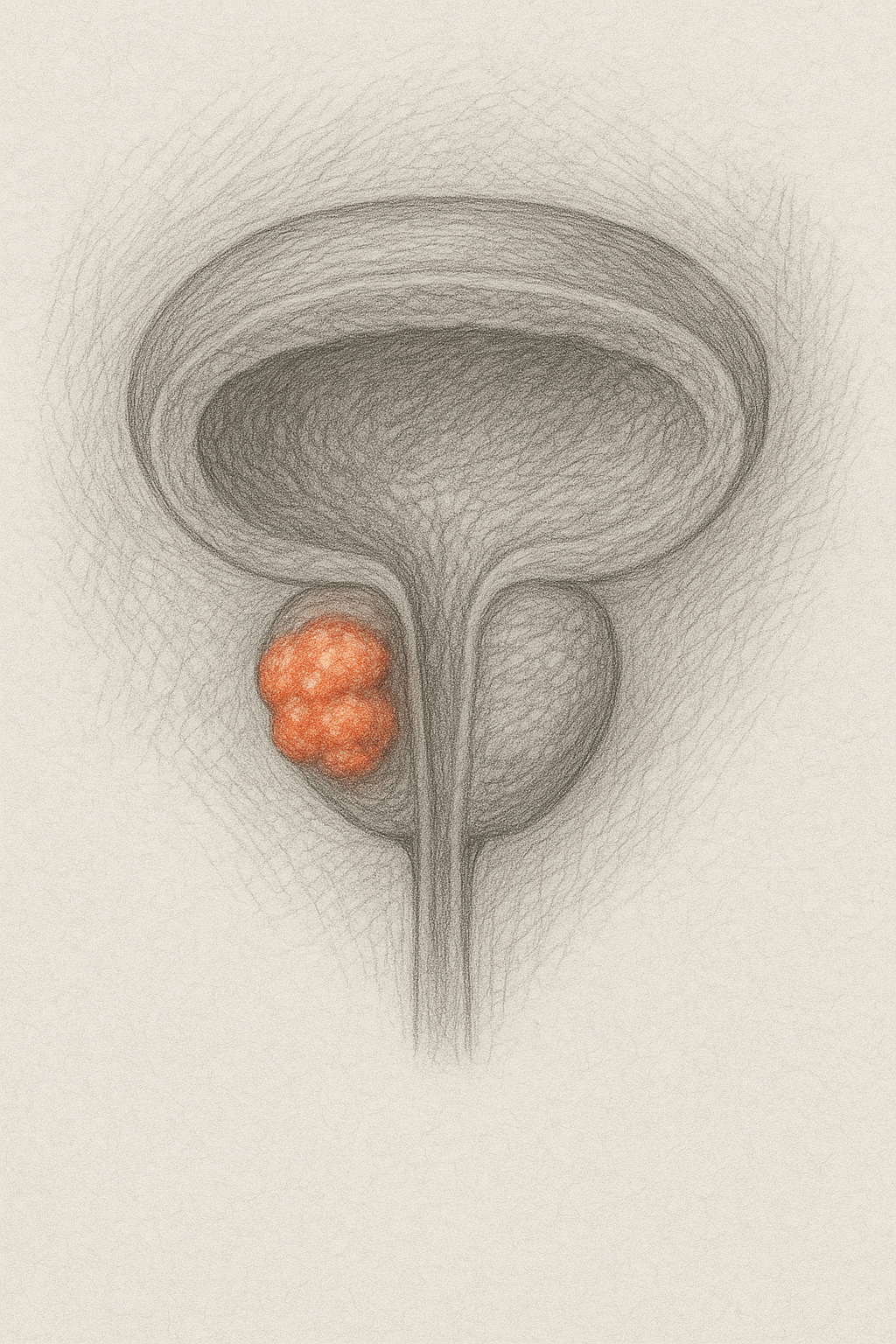
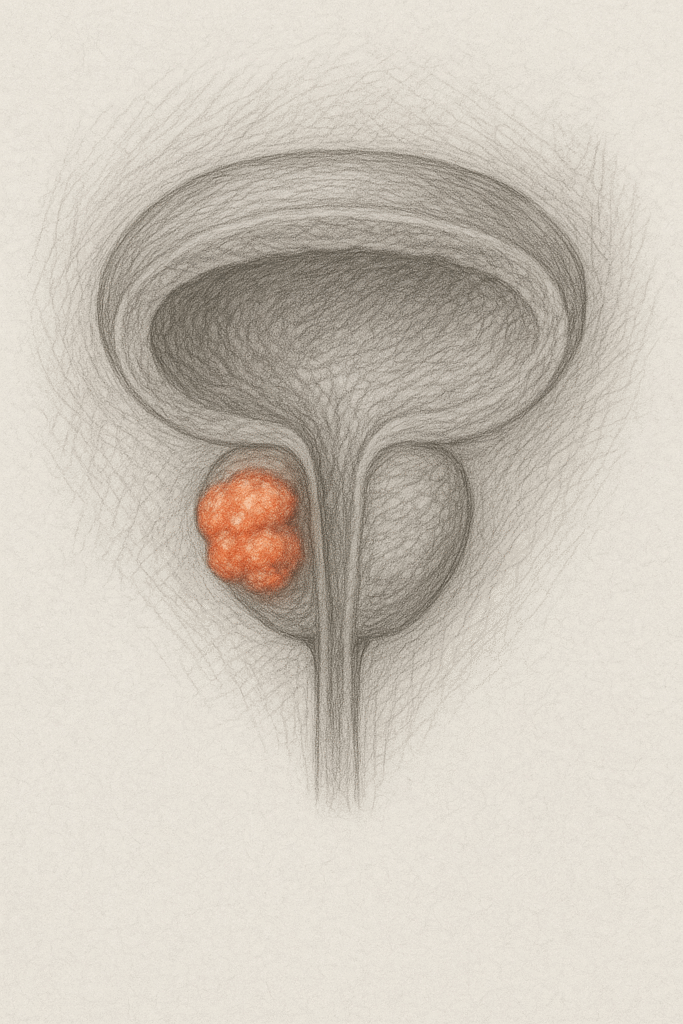
Study Design & Population
- Retrospective cohort study using VHA database (2017-2024)
- 4,890 male veterans with mCSPC initiating first-line ADT-based therapy
- Median age 74 years; 57.6% White, 28.5% Black
- Treatment groups: ADT alone (47%), ADT + ARPI (40%), ADT + NSAA (7%), ADT + docetaxel ±other (6%)
- Median follow-up: 24.7 months (PSA follow-up: 14.6 months)
Key Findings
- 44% of patients achieved PSA <0.2 ng/mL; 74% achieved ≥90% PSA decline
- PSA <0.2 ng/mL (vs not achieving): HR 0.46 for death, HR 0.45 for progression
- ≥90% PSA decline: HR 0.78 for death, no significant benefit for progression
- ADT + ARPI achieved PSA <0.2 ng/mL more frequently than ADT alone (53% vs 39% over entire follow-up)
- 42% of ADT + ARPI vs 23% of ADT-only patients reached target within 9 months
Clinical Implications
- Redefine treatment success from percentage PSA decline to absolute PSA nadir <0.2 ng/mL
- Consider combination therapy (particularly ADT + ARPI) for patients not achieving PSA <0.2 ng/mL
- Monitor PSA trajectory closely in first 9 months to identify patients needing treatment intensification
Limitations
- Retrospective design with potential selection bias and unmeasured confounders
- Veterans population may limit generalizability to broader patient demographics
- Variable follow-up periods and missing data on disease volume/risk stratification
- No randomized comparison of treatment strategies based on PSA response thresholds